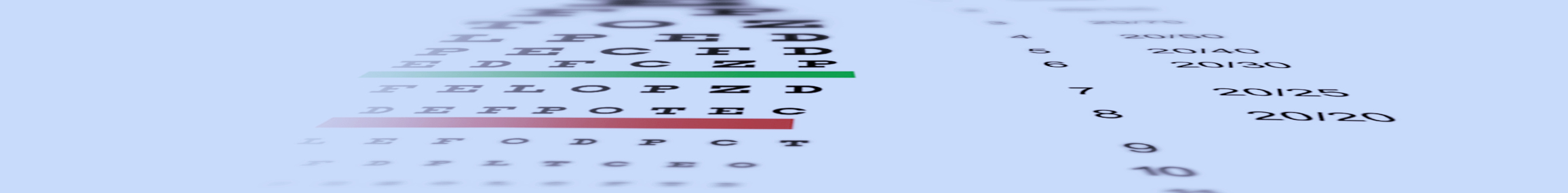
It is important for any patients with diabetes (type 1, type 2, or latent autoimmune diabetes) to have annual eye exams as they are at an increased risk of developing many eye conditions and complications. Early detection of any potential problem will lower the risk of vision loss from diabetes. The doctors at Koetting Eye Center are trained using the latest technology to detect and monitor the earliest signs of diabetic eye disease.
In what ways can diabetes affect one’s eyes?
- Blurred vision: When uncontrolled, fluctuations in blood sugar can cause quick changes in glasses or contact lens prescriptions. This is because a higher concentration of sugar inside the natural lens of the eye causes swelling of the lens. It is important that eyeglasses and contact lenses are not prescribed in patients experiencing high fluctuations in blood sugar, as the prescription is likely to change once the blood sugar is controlled.
- Cataracts : It is common for patients with diabetes to develop cataracts at a younger age than average. Symptoms include: blurred or cloudy vision, poor color contrast, glare, and difficulty driving at night.
- Glaucoma: As blood vessels weaken from diabetes, new blood vessels may form in an effort to restore blood flow throughout the eye. In rare cases, these blood vessels will block the area that drains fluid from the eye, resulting in an increase in eye pressure. If left untreated, elevated eye pressure can damage the optic nerve and cause permanent vision loss.
- Diabetic retinopathy
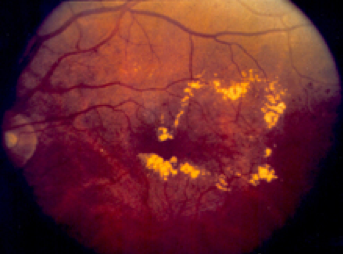
Diabetes is a condition that affects the small blood vessels in the body. Over time, the disease causes the walls of these blood vessels to weaken, eventually allowing fluid and blood to leak outside of the blood vessels. The retina is especially susceptible to this leaking because it has a high concentration of small blood vessels. Damage to the retina from diabetes is termed diabetic retinopathy and is a leading cause of blindness in adults. In most cases, this is completely preventable with close monitoring and tight blood sugar control. Early stages of diabetic retinopathy usually has no symptoms; which makes it so important for patients with diabetes to have annual exams. As diabetic retinopathy progresses, it can be divided into two categories: nonproliferative (NPDR) diabetic retinopathy and proliferative diabetic retinopathy (PDR).
Nonproliferative diabetic retinopathy is the earlier, less severe form of diabetic retinopathy. This occurs when the retinal blood vessel walls begin to break down and allow fluid or blood to leak into the retina. The location of the leaking blood vessels determines if the vision will be impacted. Fluid leaking in an area called the macula is termed diabetic macular edema. Diabetic macular edema is treatable using injectable medication and laser treatment, but the best outcomes come when detected early.
Proliferative diabetic retinopathy occurs when new, abnormal blood vessels grow in the retina. These blood vessels are brittle and cause many problems in the eye, including severe vision loss from leaking vessels and retinal detachments. Depending on the severity, PDR is usually reversible and vision loss is preventable with injectable medication and laser treatment.

Your role in reducing the risk of diabetic eye disease
Blood sugar control is the best way to prevent vision loss from diabetes. Diet, exercise, and medical management by an endocrinologist are the best ways to keep your blood sugar under control. It is imperative to schedule an annual eye exam with a thorough retinal examination. Ocular conditions associated with diabetes have a much better prognosis when detected early. Call us today to schedule your annual diabetic eye exam.