The clear front surface of the eye is called the cornea and is responsible for focusing light to the back of the eye. Keratoconus is a condition that causes a thinning and forward bulging of the cornea, affecting one’s ability to focus light and see properly. A study in the Netherlands found the number of people living with the disease to be as high as 1 in 375. Keratoconus typically begins to cause changes to the cornea in the teens, is most often diagnosed in the 20’s, and progresses through the early 40’s. As the disease progresses, eye glasses no longer provide satisfactory vision and specialty contact lenses are required. Specialty contact lenses, such as scleral lenses, recreate a smooth surface to the front of the eye so light can focus again. Advancements in technology allow us to diagnose keratoconus at an earlier age. Treatment options have also dramatically improved in the recent years, so early detection and intervention are more important than ever.
Causes of Keratoconus
Despite significant research, not a lot is known about exactly what causes keratoconus. Some research suggests that it is a genetic condition and can be passed down to family members. Those that have keratoconus have excessive enzymes that breakdown and weaken the collagen fibers in the cornea, allowing it to protrude forward. Family members of those with keratoconus are at higher risk of having too much of this enzyme.
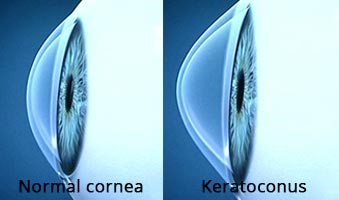
Others associate keratoconus with allergic conditions such as chronic allergies and eczema. Vigorous eye rubbing that is common in patients with allergic conditions can also weaken the fibers in the cornea that allow it to keep is round shape. For this reason, those who have been diagnosed with or those with high-risk for keratoconus should avoid excessive eye rubbing.
Connective-tissue disorders have been linked to an increased risk of keratoconus as they can cause weakening of the connective tissue within the cornea. Examples include Ehlers-Danlos syndrome, osteogenesis imperfecta, mitral valve prolapse, Marfan syndrome, etc.
Symptoms of Keratoconus
Symptoms of keratoconus are often first experienced in the late teens and worsen as the condition progresses. Symptoms vary but often include:
- Blurry vision
- Distorted vision
- Nighttime glare
- Nearsighted and astigmatism
- Poor vision with new glasses
- Frequent prescription changes
- Poor vision with soft contact lenses
- Discomfort with contact lenses
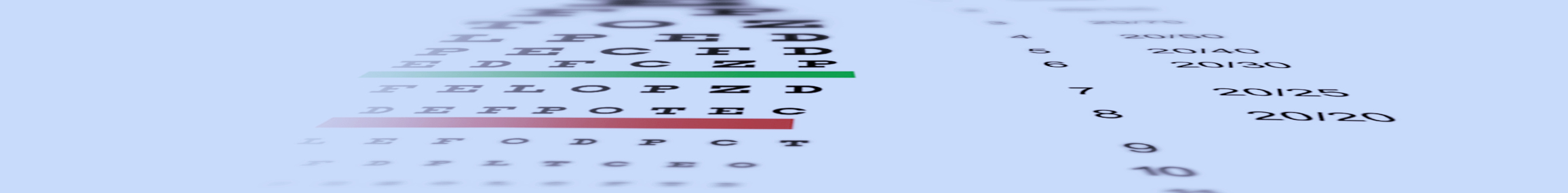
How is Keratoconus Diagnosed?
There are a handful of diagnostic tests and procedures that can aid in the diagnosis of keratoconus. While corneal mapping is essential to confirm the diagnosis, all the following tests are useful as they provide information on the severity and long-term outcome of the disease.
Refraction: A procedure done to determine a glasses or contact lens prescription, and monitor changes to these prescriptions over time.
Slit Lamp Examination: A specially designed, high-powered, microscope is used by an eye care professional to visualize the front surface of the eye and examine all layers of the cornea related to keratoconus.
Corneal mapping: Also known as corneal topography, corneal mapping scans the front surface of the eye and creates an elevation map of the cornea. It also highlights areas that have excessive curvature, which is characteristic of keratoconus.
Corneal thickness measurements: The thickness of the cornea can be measured with a scanning laser or ultrasound technology and compared over time. Progressive corneal thinning can be an indication of keratoconus.
Rigid Lens Acuity Test: A rigid surface contact lens is applied to the surface of the eye. If the patients vision improves compared to their glasses prescription, they may have an irregular cornea because of keratoconus.
Treatment for Keratoconus
In the early stages, keratoconus can be treated with glasses and soft contact lenses. As the disease progresses and the cornea becomes more irregular, rigid contact lenses become the mainstay treatment. Most patients with keratoconus do not progress beyond this point. However, some patients continue to advance to corneal thinning and scarring that does not correct well with contact lenses and a corneal transplant is needed.
Specialty contact lenses options include:
Custom soft contact lenses: Mild to moderate keratoconus can be managed with custom soft contact lenses. Today’s technology allows for the manufacturing of specialty soft contact lenses with virtually any prescription.
Rigid gas permeable contact lenses (RGPs): Commonly referred to as hard lenses, RGPs are an excellent choice for mild to moderate keratoconus. Typically, they provide better vision than soft lenses as they can reshape the irregular surface of the cornea created by keratoconus. As the keratoconus progresses, it may become difficult to maintain proper lens fit and keep the lens from falling off the eye because of its relative small size. Contact lens comfort can also become an issue.
Piggyback contact lenses: A small diameter hard contact lens is worn over a soft contact lens. This contact lens fitting design has the visual benefits hard lenses and the comfort of soft contact lenses.
Hybrid contact lenses: These lenses have a hard contact lens center attached to a soft contact lens skirt. As in piggyback lenses, hybrid contact lenses are designed to provide the vision of hard lenses with the comfort of soft contact lenses. Advancements in hybrid contact lens technology now allows for the fitting of all stages of keratoconus.
Scleral contact lenses: These are large diameter hard contact lenses that provide clear and comfortable vision. Scleral contact lenses are unique in that they never touch the cornea. They vault over the cornea and gently rest of the white part of the eye, or sclera, as their name implies. Scleral lenses tend to be very comfortable and stable on the surface of the eye because of their large size. They are available in a variety of shapes and sizes, meeting the needs of “normal” eyes all the way to severe keratoconus or corneal transplants.
Surgical Treatment for Keratoconus
Keratoconus surgical procedures do not eliminate the need for specialty contact lenses. While it may be easier to wear contact lenses after surgery, most of the time they will still be required to achieve optimal vision.
Collagen cross-linking (CXL): Until the advent of collagen cross-linking, surgery for keratoconus usually meant a corneal transplant. This was a last resort because of the associated complications. These patients were fit with specialty contact lenses until vision was no longer satisfactory and a corneal transplant was necessary to maintain quality of life. Today, collagen cross-linking should be considered a first-line therapy in patients with progressive keratoconus.
Although collagen cross-linking has been around for over a decade in other countries, it was not FDA approved in the United States until 2016. As keratoconus progresses it thins and weakens the cornea, which over time causes it to bulge forward. Collagen cross-linking is a minimally invasive procedure is performed to strengthen the cornea and arrest these changes. This may improve vision in some patients and lessen the likelihood of a future corneal transplant.
Collagen cross-linking is performed with riboflavin (vitamin B2) eye drops and ultraviolet light. The procedure is done one of two ways: epithelial-on or epithelial-off. Typically, epithelial-on takes longer to perform but is associated with fewer complications.
Intacs: Originally introduced to correct low amounts of nearsightedness, intacs are now used to treat irregular corneal surfaces, such as keratoconus. They are surgically implanted into the outer edge of the cornea to flatten and create a more regular surface. These are of similar material to rigid contact lenses and cataract surgery implants. In patients with keratoconus, intacs can make it easier to tolerate contact lens wear and improve the vision with glasses. Some surgeons are finding success coupling collagen cross-linking and intacs in one procedure. To achieve the best vision possible, specialty contact lenses are still required by almost all patients with keratoconus.
Corneal transplantation: When corneal scarring from keratoconus causes vision loss this is not correctable with specialty contact lenses or glasses and a corneal transplant may be necessary. In this procedure, the diseased cornea is surgically replaced with a healthy donor cornea. Corneal transplants are performed a variety of ways, from a partial thickness to a full thickness transplant. Depending on the procedure, the healing process varies among patients, ranging from a few weeks to a year or more. The most appropriate corneal transplant procedure will be determined on an individual basis.
Although corneal transplantation is a relatively safe procedure, there are serious risks that need to be considered before the procedure is performed. Graft rejection is a complication that occurs when the body’s own immune system attacks the donor cornea. This has been reported in 10% of corneal transplants and requires steroid eye drops or a second transplant. It is always best to first attempt to improve vision with specialty contact lenses before a corneal transplant to minimize risks of complications.