Dry eye is a chronic and typically progressive condition. Around one third of the U.S. population will be affected by dry eye at some point in their lifetime. Although dry eye can affect individuals at any age, symptoms are often worse for those over forty-five years old. Symptoms can range in severity from a mild annoyance to extreme debilitation. There are many types and causes of dry eye, and because of this, it is important to develop a customized treatment approach to address the specific cause.
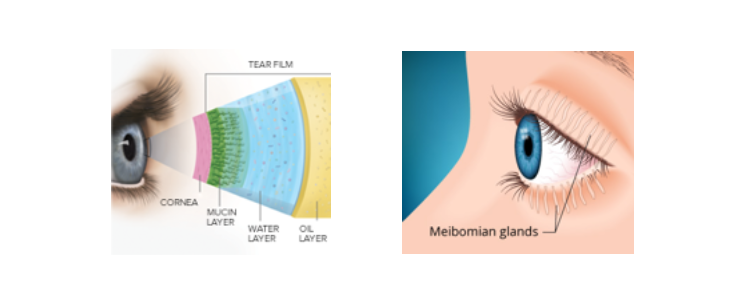
To understand dry eye, it is important to understand how tears work. Our tears, also known as the tear film, are comprised of three layers: mucous layer, watery layer and oily layer. The mucous layer is the closest to the eye and responsible for allowing the tears to spread over the surface of the eye. The watery layer, or aqueous layer, is the thickest layer of the tear film and is responsible for providing hydration and nutrients to the surface of the eye. Lastly, the outermost layer is called the oily or lipid layer of the tear film. It functions to prevent the evaporation of the underlying layers of tears. It essentially creates an oil slick over the surface of the tears. Without the oily layer of tears, the tears would evaporate instantaneously, causing discomfort and blurry vision. These oils are secreted by the meibomian glands of the eyelids, therefore, when these glands are not functioning properly, it is called meibomian gland dysfunction (or MGD). Studies tell us that MGD is present in 86% of dry eyes.
By examining the quantity and quality of tears, eyelids and surface of the eye, the exact cause of dry eye can be determined, and the most appropriate treatment plan can be put into place.
What Causes Dry Eye?
Dry eye is “multifactorial”, which means it involves or is dependent upon a number of factors or causes. Underlying causes of dry eye include everything from the environment around us to our general health. Specifically, dry and dusty environments, forced air in cars, buildings and airplanes; post-menopausal hormonal changes, medical conditions such as autoimmune diseases, rosacea, diabetes and thyroid disorders; prescription medications, facial products and makeups, LASIK eye surgery, digital device use, improper blinking and eyelid positioning all can cause symptoms of dry eye. It is important to determine the exact cause to create the most effective treatment plan.
Symptoms of Dry Eye
Symptoms of dry eyes and dry eye syndrome include:
- Burning sensation
- Itchy eyes
- Aching sensations
- Heavy eyes
- Fatigued eyes
- Sore eyes
- Dryness sensation
- Red eyes
- Photophobia (light sensitivity)
- Blurred vision
- Stringy mucus in or around your eyes
- Contact lens intolerance
- Tired eyes
Another common symptom is foreign body sensation — the feeling that grit or some other object or material is "in" your eye.
And as odd as it may sound, watery eyes also can be a symptom of dry eye syndrome. This is because dryness on the eye's surface sometimes will over-stimulate production of the watery component of your tears as a protective mechanism. But this "reflex tearing" is different than the normal tears and does not stay on the eye long enough to correct the underlying dry eye condition.
How is Dry Eye Diagnosed?
Dry eye disease can be diagnosed by an eye doctor at an in-office examination. The doctor or technician will perform specific tests and procedures based on the patient’s symptoms and the results of the eye examination. The results of these tests will tell the doctor if dry eye is present, the severity of dry eye disease, underlying causes and the best treatment approach. Specific dry eye diagnostic tests include:
Slit Lamp Examination: A specially designed, high-powered, microscope is used by an eye care professional to visualize the surface of the eye, examining all structures that could relate to dry eye disease.
TBUT (Tear Break Up Time): This evaluates the quality of tear production by measuring the amount of time it takes for the tears to evaporate off the surface of the eye.
Schirmer’s Test: Filter paper is placed on the inside of the lower eyelid. Based on the amount of tear absorbed by the filter paper in a five minute period, the quantity, or volume of tears, can be determined.
Meibography: A high-definition scan of the oil-producing meibomian glands of the eyelid is used to visualize these glands. Diseased and clogged glands can be detected and treated before total gland loss occurs. This is critical as meibomian gland disfunction (MGD) is the number one cause of dry eye.
Fluorescein Eye Staining: A dotting paper containing fluorescein dye will be touched to the surface of the eye. As the patient blinks, the dye should spread evenly over the surface of the eye. Your eye care provider will then shine a blue light on the surface of the eye. Areas of dry eye related irritation will then appear highlighted.
MMP9 Testing: A sample of the patient’s tears are collected and evaluated for matrix Metallopeptidase 9 (MMP9). Levels of MMP9 are elevated in patients with eye inflammation related to dry eye disease.
Treatment Options for Dry Eye
There is no one treatment option that works for every patient. The goal of treating dry eye disease is to not only treat the symptoms, but to correct the underlying cause. A clinical examination and dry eye evaluation will determine the most effective treatment plan. Dry eye treatment options include:
Lubricating Eye Drops: There are a wide variety of over-the-counter lubricating agents available. Thickness, or viscosity, of the lubricating drops varies among brands. There are also gels and ointments that last longer than standard drops. Some drops are oil-based while others are water-based. In general, it is best to use a preservative free version if available. An eye doctor can determine the most effective lubricating drop based on the cause of the dry eye disease.
Restasis & Xiidra: These are both prescription eye drops designed for patients with dry eyes. Restasis works by reducing eye inflammation associated with dry eye disease and helps the body produce more natural tears. Xiidra has been FDA approved to treat the signs and symptoms of dry eye disease. Both medications need to be used for a minimum of 90 days to experience their full effect.
Steroid Eye Drops: Patients with moderate to severe dry eye are often treated with steroid eye drops to quickly relieve discomfort. These are mild corticosteroids that are used only for a short-term (typically weeks to months) to minimize side effects that can be associated with steroid eye drops. It is often necessary to treat dry eye inflammation prior to or in conjunction with other treatment options.
Eyelid Cleansers and Warm Compresses: Lid hygiene is an essential part of any dry eye treatment regimen. Dandruff-like byproducts of bacterial overgrowth can accumulate on the eyelids and lashes. The debris then falls into the eyes throughout the day, resulting in redness and irritation. This also creates inflammation and blockage of the oil-producing meibomian glands on the eyelids. A hypochlorous acid-based spray or cloth can be used to remove these microorganisms and debris from the lids and lashes. In addition, a warm compress used for 5-10 minutes helps loosen the blockages within the meibomian glands and maintain normal gland function. For best results, eyelid cleansers and warm compresses should be performed 1-2 times daily.
Nutritional Supplements: Data suggests omega-3 fish oil supplementation may be an effective therapy for managing dry eye disease and meibomian gland dysfunction. The benefits stem from the anti-inflammation effects of fish oil to help reduce dry eye related inflammation. Daily recommended dosage of omega-3 fish oil varies among patients and depends on the severity of the dry eye disease. Caution should be taken in patients on blood thinners as high doses of omega-3 fish oil might keep blood from clotting and increase the risk of bleeding.
Tear Duct Plugs: Patients who do not produce enough tear will benefit from tear duct plugs, also known as punctal plugs. This is a simple in-office procedure that take minutes to perform. In patients with dry eye, not enough tear is being held on the surface of the eye. The little tear they do have is drained through a small opening on the insider corner of the eyelids called the puncta. A punctal plug can be placed over the tear duct opening, slowing the drainage of tears and holding more of the natural tear on the surface of the eye. In addition, punctal occlusion allows the effect of lubricating eye drops to last much longer and work more effectively, as they are not drained from the surface of the eye as quickly.
LipiFlow: When meibomian gland dysfunction is the cause of dry eye disease, LipiFlow is a very effective treatment. This 12-minute in-office treatment is designed to remove blockages from the meibomian glands, allowing them to properly function and produce the oils that make up the top protective lipid layer of the tear film. LipiFlow safely and comfortably delivers a combination of heat to the inner lids and simultaneous therapeutic motion to the outer lids, removing blockages from the meibomian glands. After the initial numbing drops, the LipiFlow procedure offers a drug-free mechanism of action. Removing blockages allows the glands to resume production of oils or lipids. This oil is essential for a healthy tear film, stable vision, and ocular comfort. Maximum results are usually experienced 6-8 weeks after treatment.
Please call today to schedule an evaluation with one of Koetting Eye Center's dry eye specialists.
Dry Eye and MGD? (with subtitles) from TearScience on Vimeo.